After 9 months of trying different approaches and countless hours of research, I gained valuable insights into the donor sperm journey.

When I first started exploring getting pregnant with a sperm donor, I felt overwhelmed by the choices: home insemination vs. medical clinics, anonymous vs. known donors, and the maze of legal considerations.
After months of trying different approaches and countless hours of research, I gained valuable insights into the donor sperm journey. Now I want to share everything I learned along the way – the practical stuff that actually matters when you’re navigating this journey in the UK.
This guide breaks down exactly what you need to know, based on extensive research and the experiences of countless women who have walked this path (sometimes learning things the hard way).
After trying home insemination, some people find they need additional medical support. What I discovered was that there are multiple clinical paths to conception with donor sperm, each offering more intensive intervention when home methods haven’t been successful.
Many people start their journey with at-home insemination because they want to try the most natural, comfortable approach first. Many people succeed with this method before needing to consider clinical options, and the relaxed environment of your own home can actually improve your chances of conception.
It is important to note that in the UK, sperm purchased from licensed sperm banks (even overseas ones) cannot legally be shipped directly to your home for insemination.
By law, donor sperm must be used within a licensed fertility clinic to ensure safety, proper screening, and legal protections for all parties involved. Home insemination with donor sperm from a clinic is therefore not allowed. So if you’re considering home insemination, you’ll need to find a known donor.
NOTE: Working with known donors requires careful legal consideration. We recommend establishing clear agreements from the outset, as circumstances can shift once a baby arrives. We’re developing comprehensive guidance on known donor agreements and will be linking to detailed legal resources soon.
Locating a known sperm donor can be accomplished through two main avenues: reaching out to someone within your personal network or utilising specialised matching platforms. Your personal network might include trusted friends, acquaintances, or relatives who are willing to help. Alternatively, you can explore online platforms designed to connect prospective parents with willing donors.
Donor match-making services to consider:
These platforms facilitate connections between intended parents and potential donors who are open to being known rather than anonymous.
When working with a known donor, establishing clear, honest dialogue is essential. You’ll need to navigate important legal frameworks and ethical questions together, while also ensuring the donor completes all required health screenings and medical evaluations.
At-home insemination involves the use of a needleless syringe to deposit a sperm sample into the vagina, positioned close to the cervix.⁷ You can learn more about intracervical insemination (ICI) on the Tily Blooms website.
A typical step-by-step process looks like this:
1. Medical Consultation
It is strongly recommended to consult with a medical professional prior to attempting at-home insemination.⁸
My GP was supportive, and I had what is known as a Fertility MOT, which cost around £400 in 2020. It’s a comprehensive assessment of a woman’s reproductive health, designed to identify potential issues affecting her ability to conceive. The MOT involves a range of tests and examinations to evaluate ovarian reserve, uterine health, and overall reproductive function. It’s done mostly privately in the UK, but check with your doctor to see if the NHS offer them.
2. Finding Donor Sperm
Obtain donor sperm from what is called a known donor. As mentioned above, there are websites that offer donor matching services. This is a great place to start.
3. Creating Your Space
I transformed my bedroom into a calm sanctuary with soft lighting and relaxing music. Having my own space made such a difference to my mindset.
4. Tracking Your Cycle
The most fertile period typically spans 12-24 hours around ovulation.⁸
You can use paper strip tests (like the ones that Tily Blooms includes in the complete kit), so you can track your ovulation cycle on the A4 sheet inside the Tily Blooms Fertility Tracking Journal.
For detailed guidance, see How to Read an Ovulation Test: Your Complete Guide on Tily Blooms.
5. The Actual Insemination
On ovulation day, using a Tily Blooms fertility wand, the process involves slowly depositing the sample near the cervix whilst lying with hips elevated.
The At Home Insemination Guide from Tily Blooms provides invaluable guidance during this process.
6. The Wait
Many women find it helpful to stay lying down for around 40 minutes to an hour, gently shifting positions every 10 minutes. Then comes the two-week wait!
For individuals with no known fertility concerns, home insemination success rates are approximately 10-15% per cycle.⁸
Many people find success in 3 to 4 cycles.

The Tily Blooms Home Insemination Kit (Complete Kit) is designed to facilitate at-home insemination, providing essential tools for two inseminations.⁹
This comprehensive kit includes two round-headed fertility wands (syringes), two collection cups, ten ovulation tests, five pregnancy tests, two urine collection containers, two tubes of semen-friendly lubricant, two soft cervical discs, and an instruction manual.⁹
Understanding the differences between sperm types and procedures can help you make informed decisions about your conception journey:
| Type of Sperm | Procedure | Lifespan in Body | Notes |
| Frozen (washed) | IUI/Home Insemination | 12–24 hours | More fragile post-thaw |
| Fresh (washed) | IUI | 24–72 hours | Longer lifespan than frozen |
| Fresh (unwashed) | Home Insemination | Up to 5 days | Protected by natural seminal fluid |
Unlike IUI, which bypasses the cervix and places lab-washed sperm directly into the uterus, home insemination allows sperm to interact naturally with cervical mucus.
This mucus plays a key role in filtering and guiding the healthiest sperm toward the egg, while also protecting and nourishing them.
As a result, fresh sperm used in home insemination can survive in the body for up to five days — significantly longer than frozen sperm used in IUI, which typically lives for only 12 to 24 hours.
Home insemination offers a gentler, less clinical approach by working in harmony with the body’s natural processes, with a strong chance of success when timed correctly!
It’s also worth exploring IUI at a fertility clinic. Intrauterine insemination (IUI), also known as artificial insemination, is a fertility procedure designed to facilitate conception by directly placing sperm into the uterus around the time of ovulation.¹
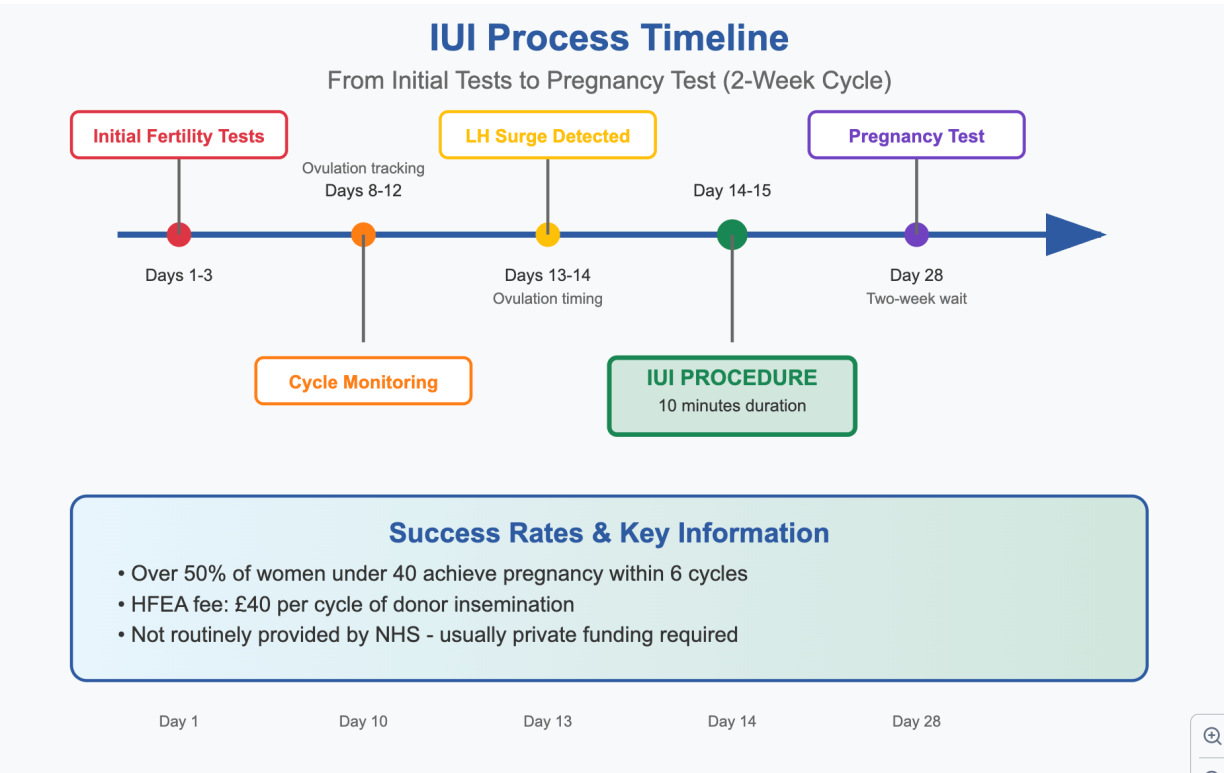
The IUI process breaks down into these key stages:
Initial Fertility Tests
Before commencing IUI, individuals undergo fertility assessments to confirm the procedure’s suitability. These tests include verifying that the fallopian tubes are open and healthy.¹ Expect to spend about £300 on these initial tests, which will give peace of mind that IUI would work for your body.
Timing with Ovulation
IUI is precisely synchronised with the recipient’s ovulation.¹
I tracked my cycle religiously using ovulation tests and found my LH surge typically happened between day 12-15.
It’s VERY important to pinpoint ovulation using strips rather than just tracking on an app, as the days vary month to month.
I can’t stress this enough and is a reason many don’t conceive, as they track using an app rather than ‘manually’.
The Procedure
The IUI procedure itself is typically brief, lasting no more than 10 minutes.¹ It’s often described as feeling similar to a smear test – slightly uncomfortable but not painful.
Success Rates
Over half of women under 35, many undergoing IUI achieve pregnancy within six cycles.¹
IUI is not often recommended to women over 35, and the stats are relatively low after this age.
The cost reality can be significant though. IUI is not routinely provided by the National Health Service (NHS).¹
Expect to pay approximately £1,200 per cycle at a private clinic, plus anywhere between £800-£1200 for donor sperm each time. The Human Fertilisation and Embryology Authority (HFEA) levies a £40 fee for each cycle of donor insemination.¹
IVF is typically recommended for individuals who face significant challenges in conceiving, particularly when both home insemination and IUI have been unsuccessful, or when there are known conditions such as blocked fallopian tubes, severe endometriosis, or other substantial fertility issues.
| Feature/Aspect | IUI with Donor Sperm | At-Home Insemination (ICI) with Donor Sperm |
|---|---|---|
| Method Type | Intrauterine Insemination | Intracervical Insemination |
| Location | Fertility Clinic | Home |
| Invasiveness | Moderately invasive (catheter into uterus) | Non-invasive (syringe into vagina, near cervix) |
| Medical Supervision | Required | Recommended (initial consultation crucial) |
| Sperm Preparation | Washed & Concentrated (removes impurities) | Not washed |
| Success Rates (per cycle) | 10-20% (varies by age, fertility factors)⁴ | 10-15% (similar to natural intercourse)⁸ |
| Cost Implications | Higher (NHS funding limited, often private)¹ | Lower (cost of sperm + kit)⁸ |
| Suitability (for whom) | Same-sex couples, single individuals, unexplained infertility, mild male factor, mild endometriosis¹ | Same-sex couples, single individuals, unexplained infertility, mild male factor, mild endometriosis, and individuals with no known fertility issues⁸ |
| Typical Cycles to Conceive | Over half under 40 within 6 cycles¹ | Several attempts often needed⁸ |
| Key Advantages | Higher success rates for some conditions, professional medical oversight, precise timing | Comfort, privacy, affordability, less clinical environment |
| Key Disadvantages | Higher cost, clinic visits, potential discomfort, risks with ovulation stimulation | Lower success rates for fertility challenges, requires careful self-management, risks if donor not screened or fertility issues undiagnosed |
Recommendation: For individuals with no known fertility issues, starting with at-home insemination (ICI) allows you to try the most affordable, comfortable method first. You can always progress to clinical methods if needed.
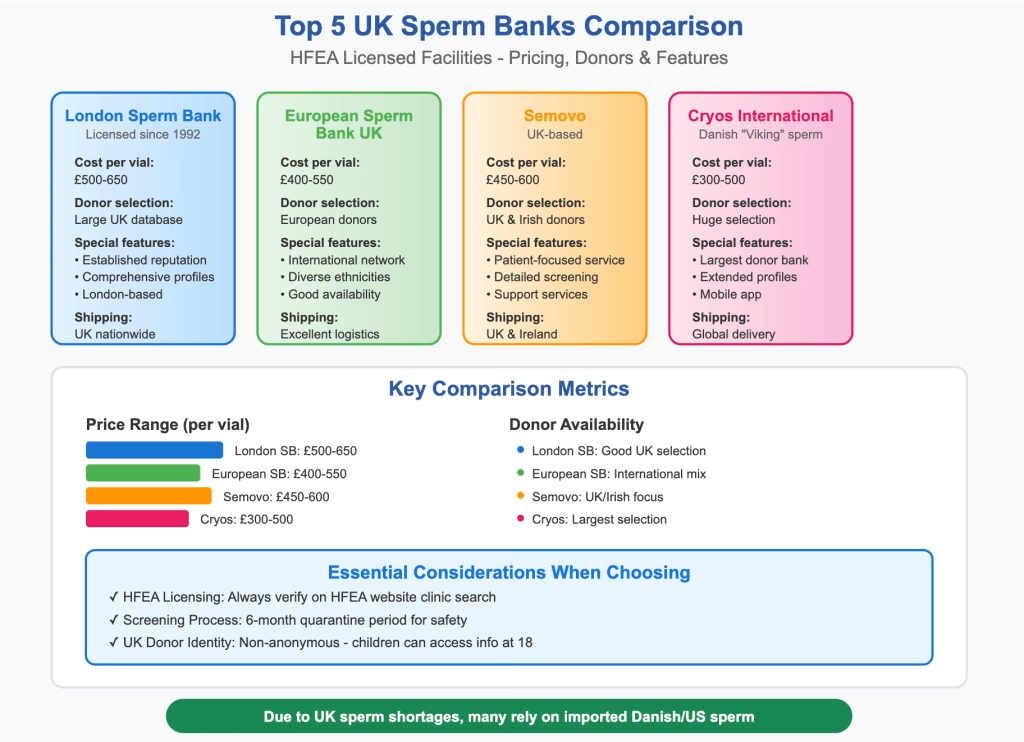
In the UK, sperm banks must be licensed by the Human Fertilisation and Embryology Authority (HFEA).¹⁵
The major UK banks include London Sperm Bank (licensed since 1992), European Sperm Bank UK, and Semovo. Many UK clinics also import sperm from Danish banks like Cryos International and European Sperm Bank Denmark.
What really matters when choosing a bank:
HFEA Licensing
Always verify the bank is HFEA-licensed. You can check this on the HFEA website’s clinic search function.
Screening Process
All donors must pass screenings for infectious diseases in HFEA-approved laboratories.⁵ The 6-month quarantine period may seem frustrating at first, but it’s essential for safety.
Available Information
UK donors cannot be anonymous – at age 18, donor-conceived children can access identifying information.¹⁰ This was actually reassuring to me, knowing my future child would have that option.
Family Limits
Licensed clinics are expected to adhere to the ’10-family limit’, which restricts the number of families that can be created with a single donor through fertility treatment in the UK.⁹ Many people appreciate this lower limit compared to some countries.
Storage and Shipping
Check their shipping success rates and storage options.
I created a spreadsheet (yes, really!) with these categories:
Physical Traits
I looked for someone with similar colouring to me – brown hair, green eyes, medium build. This felt important for family resemblance.
Health History
A thorough review of the donor’s medical history helps avoid conditions prevalent in the recipient’s own family.¹¹ If your family has a history of diabetes, you might prioritise donors with clean metabolic health.
Open ID Requirements
In the UK, donor anonymity was lifted in April 2005. Registered sperm donors in the UK must therefore agree to be identifiable.¹¹ At age 16, children can access non-identifying information, and at 18 they can obtain a donor’s last-known contact details.¹⁰
Education and Interests
Whilst not genetic, I found myself drawn to donors who shared my love of reading and outdoor activities. It helped me picture the kind of person they might be.
The legal side initially scared me, but understanding the basics helped:
Parental Rights
Under the Human Fertilisation and Embryology Act 1990, donors have no legal, financial, or social responsibility for any children born from their donation.¹⁵ Using a licensed bank ensures this protection.
This doesn’t apply if you are using a known donor or finding a donor on a match-making website.
The Reality of UK Donor Identity
Here’s what I wish someone had told me earlier: whilst legal frameworks exist, the widespread availability of genetic testing means biological connections can often be discovered regardless. It’s worth preparing for the possibility your child might find their donor or half-siblings through DNA testing.
Donor Compensation
In the UK, it’s illegal to pay a donor anything other than expenses. A person donating sperm at a licensed clinic can claim no more than £45 per clinic visit.¹³ This means UK donors are truly altruistic.
| Consideration Category | Specific Factors to Evaluate |
|---|---|
| Medical & Genetic Health | Family medical history (absence of prevalent diseases)¹¹ |
| Genetic screening results⁵ | |
| CMV status (match recipient’s status)¹¹ | |
| Physical Characteristics | Height, eye colour, hair colour, ethnicity (to match recipient/partner)⁵ |
| Identity & Relationship | UK requirement for identifiable donors⁵ |
| Understanding of future contact possibilities¹¹ | |
| Practical Logistics | Number of vials available (for future siblings)¹¹ |
| Shipping options⁸ | |
| Personal Values | Education level, hobbies, interests, personality traits (as available in profile)⁵ |
| Shared values⁵ |
Beyond the medical and logistical aspects, two things made the biggest difference in my success: precise ovulation tracking and emotional support.
I became obsessed with my cycle (in a good way!). Here’s what worked:
Tily Blooms Ovulation Tests
Testing my ovulation regulary and tracking my ovulation was honestly the key to my success. The Tily Blooms complete kit comes with plenty of these!
Cervical Mucus Monitoring
Around ovulation, many women notice egg-white cervical mucus. This natural sign can confirm your tests are accurate. ¹²
Basal Body Temperature
Tracking this for three months helps you understand your pattern. The temperature rise after ovulation helps confirm timing for future cycles.
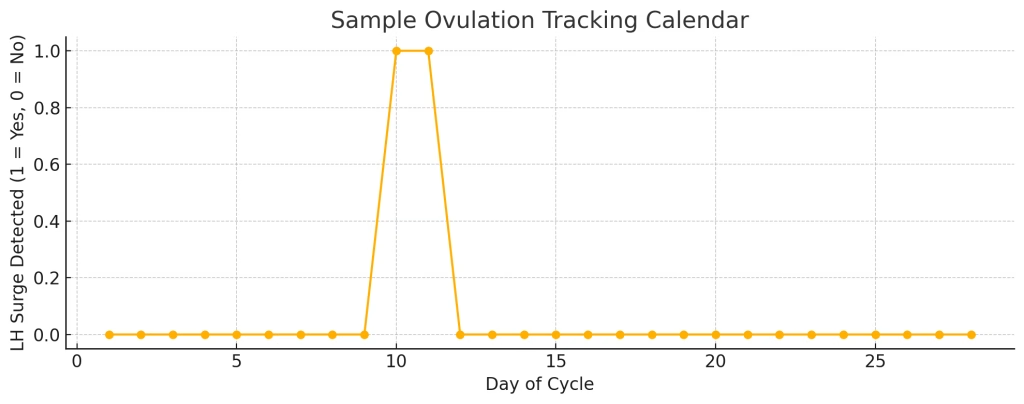
For more detailed information, see the Ovulation and Fertilisation Process guide on Tily Blooms.
The emotional rollercoaster of trying to conceive with donor sperm can catch many people off guard. What often helps people cope:
Building A Support Network
Join online forums specifically for people using donor sperm. Connecting with others who understood the unique aspects of this journey can be invaluable. The TWW Survival Planner from Tily Blooms can help navigate those difficult two-week waits.
Therapy
Finding a therapist who specialises in fertility issues can be incredibly helpful. They can work through feelings about using donor sperm and prepare for future conversations with your child.
Stress Management
Strategies such as gratitude journaling, mindfulness practices, and positive visualisation exercises can be immensely beneficial in navigating these emotional challenges.¹³ The Gratitude Journal approach recommended by Tily Blooms can be particularly helpful.
Dealing with Failed Cycles
Each negative test hit hard. I learned to plan something nice for test day – either to celebrate or to comfort myself. Having that plan reduced anxiety.
For most people with no known fertility issues, home insemination is an excellent first step. It’s cost-effective, allows you to learn your body’s patterns, and gives you control over your environment. Consider starting here if:
It’s worth a try even if you have encountered issues. You can always move to clinical methods if home insemination doesn’t work after 4-6 attempts.
Initial Fertility Assessment
Even though I planned to try at home, getting basic fertility tests first was encouraging. Knowing my tubes were open gave me confidence to proceed.
Legal Consultation
Consider paying for one session with a family lawyer to understand your rights and your future child’s rights regarding donor conception.
Ongoing Support
I maintained regular check-ins with my GP throughout the process. Having medical backup gave me confidence and peace of mind.
The UK donor sperm landscape has some unique challenges:
Sperm Shortages
Demand increasingly outstrips supply, resulting in growing reliance on imports of sperm from Denmark and from the EU.¹¹
NHS Funding
Some eligibility may exist for same-sex couples or single women, contingent upon factors such as age and geographical location.¹
HFEA Regulations
It’s generally safer to have treatment with donor sperm at a licensed clinic. Clinics in the UK are required by law to ensure that donors, patients and any future children are protected by carrying out rigorous health tests and offering everyone involved counselling.¹³
You Can Do This!
The journey to get pregnant with donor sperm can be one of the most challenging yet empowering experiences. Yes, there can be moments of doubt, frustration, and sadness. But there are also moments of hope, excitement, and ultimately, joy.
My biggest piece of advice? Trust yourself and consider starting with the gentlest approach. Whether you begin with home insemination or need to progress to clinical methods, you know what feels right for your journey.
Take it one step at a time, be patient with yourself, and remember that many of us have walked this path before you.
Stories of success often come from those who started with home insemination – whether they succeeded on their first attempt or after several cycles, many found it was the right choice for them. Some discover they conceived in the comfort of their own space after clinical methods hadn’t worked.
All the research, planning, and waiting can lead to that moment of success. The journey to parenthood through donor conception, whilst unique and sometimes challenging, has helped create countless families!
Remember, this is your unique journey to parenthood. There’s no “right” way to do it – only the way that works for you.